Patent foramen ovale (PFO) is an embryonic defect associated with an increased risk of ischemic stroke.1 PFO closure combined with long-term antiplatelet therapy is recommended to prevent recurrent stroke in selected patients.2
SWITCH TO THE interventional VIEW For more information specific to interventional cardiology regarding PFO closure
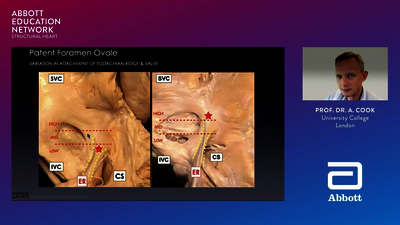
Characteristics that are strongly associated with a causal role of PFO in an ischemic stroke of unknown cause are:9
- Atrial septal aneurysm (ASA) and/or a moderate-to-severe shunt
- Atrial septal hypermobility
- PFO size
The presence of other risk factors does not exclude PFO as the causative factor, but PFO is more likely when patients are young and lack other risk factors. Determining whether a patient’s stroke is related to a PFO should involve a multidisciplinary team including a neurologist, a cardiologist, and other health professionals trained in the care of patients with stroke.4

If your patient has had an ischemic stroke of unknown cause and has also been diagnosed with a PFO, it’s important to talk to them about the benefits and risks of available treatment options to reduce their risk of another stroke.
Options that can help prevent recurrent stroke in patients who have had a PFO-associated stroke include closure of the PFO by a percutaneous device, medical therapy with antithrombotic agents, and, in rare cases, a surgical approach.
If your patient has had an ischemic stroke of unknown cause and has also been diagnosed with a PFO, it’s important to talk to them about the benefits and risks of available treatment options to reduce their risk of another stroke.
Options that can help prevent recurrent stroke in patients who have had a PFO-associated stroke include closure of the PFO by a percutaneous device, medical therapy with antithrombotic agents, and, in rare cases, a surgical approach.
PFO CLOSURE
Closure of a PFO may prevent paradoxical embolism by preventing a venous thrombus from passing through the PFO and thereby reducing the risk of recurrent stroke. Evidence from the most recent randomized controlled trials now suggests that PFO closure is effective in reducing the risk of recurrent stroke for selected patients who have had a PFO-associated stroke.
For patients who are <60 years old, have a PFO, and have experienced an ischemic stroke, PFO closure may be warranted. A critical piece in determining if a patient can benefit from PFO closure is ensuring that a comprehensive stroke workup is completed, concluding that no other evident source of stroke can be found, and the evaluation suggests that the embolism passed through the PFO.
PFO closure is a minimally invasive, catheter-based procedure that involves making a very small skin incision, guided by fluoroscopy and intracardiac echocardiography, and inserting a catheter to guide the PFO occluder through the blood vessels to close the PFO.
SHARED DECISION MAKING
Neurologists and cardiologists should discuss consideration of the PFO closure procedure, including benefits, risks, and alternative treatment options with the patient. The patient should understand the immediate and long-term potential benefits and risks of treatment options to make a well-informed decision that considers their values and preferences.
MEDICAL TREATMENT
GENERAL MEASURES
Patients with PFO who have an ischemic stroke or transient ischemic attack (TIA), who have not undergone PFO closure, should be treated with all appropriate risk reduction strategies, most importantly, antithrombotic therapy. Other measures include lifestyle modification (diet and exercise), blood pressure reduction, and statins (if indicated).
ANTITHROMBOTIC THERAPY
For most patients with an embolic-appearing stroke of unknown cause and a PFO who do not have device closure, antithrombotic therapy with antiplatelet agents is recommended.6
Another antithrombic option is anticoagulation. However, recent trials that explored anticoagulation treatment for patients with an Embolic Stroke of Unknown Source (ESUS) were negative.10 Anticoagulation is indicated for most patients with an ischemic stroke of unknown cause and PFO who have evidence of acute deep vein thrombosis (DVT), pulmonary embolism, other venous thromboembolism (VTE), or a hypercoagulable state.
SURGICAL CLOSURE OF PFO
For patients aged 60 years who have had an ischemic stroke and have a PFO with no other evident source of stroke and who have a concurrent indication for cardiac surgery, surgical closure of PFO for secondary stroke via standard or minimally invasive techniques for secondary stroke prevention may be an alternative to percutaneous PFO closure.
Most open heart surgeries are performed through an incision across the full length of the breastbone, or sternum. Open heart surgeries require the use of a heart lung machine, which takes over the function of the heart temporarily. Currently, surgery is rarely performed to close a PFO.
BACK TO WALKING 12 MILES PER DAY
As an employee of the Royal Mail postal service “I’m back on full delivery, walking nearly 12 miles a day. Now it gets to be 8:00 at night, and I’m still bouncing off the walls, full of energy. I feel that I owe everyone who was involved a massive thank you.”
Alan Butcher - England
Hub
TV
HUB
- Kent DM, Thaler DE. Is patent foramen ovale a modifi able risk factor for stroke recurrence? Stroke. 2010;41(10 Suppl 1):S26–30. doi.org/10.1161/STROKEAHA.110.595140.
- Messé SR, Gronseth GS, Kent DM, et al. Practice advisory update summary: patent foramen ovale and secondary stroke prevention. Neurology. 2020;94(20):876–885. doi.org/10.1212/WNL.0000000000009443.
- Homma S, Sacco RL. Patent foramen ovale and stroke. Circulation. 2005;112(7):1063–1072. doi.org/10.1161/CIRCULATIONAHA.104.524371.
- Mojadidi MK, Zaman MO, Elgendy IY, et al. Cryptogenic stroke and patent foramen ovale. J Am Coll Cardiol. 2018;71(9):1035–1043. doi.org/10.1016/j.jacc.2017.12.059.
- Saver JL. Clinical practice. Cryptogenic stroke. N Engl J Med. 2016;374(21):2065–2074. doi.org/10.1056/NEJMcp1503946.
- Kernan WN, Ovbiagele B, Black HR, et al. AHA/ASA guidelines for the prevention of stroke in patients with stroke and transient ischemic attack. Stroke. 2014;45(7):2160–2236. doi.org/10.1161/STR.0000000000000024.
- Homma S, Sacco RL, Di Tullio MR, et al. E ect of medical treatment in stroke patients with patent foramen ovale: patent foramen ovale in cryptogenic stroke study. Circulation. 2002;105(22):2625–2631. doi.org/10.1161/01.CIR.0000017498.88393.44.
- Elgendy AY, Saver JL, Amin Z, et al. Proposal for updated nomenclature and classifi cation of potential causative mechanism in patent foramen ovale-associated stroke. JAMA Neurol. 2020;77(7):878–886. doi.org/10.1001/jamaneurol.2020.0458.
- Pristipino C, Sievert H, D’Ascenzo F, et al. European position paper on the management of patients with patent foramen ovale. EuroIntervention.2019;14(13):1389–1402. doi.org/10.4244/EIJ-D-18-00622.
- Diener H-C, Sacco RL, Easton JD, et al. Dabigatran for prevention of stroke after embolic stroke of undetermined source. N Engl J Med. 2019;380(20):1906–1917. doi.org/10.1056/NEJMoa1813959.