Patent foramen ovale (PFO) is an embryonic defect associated with an increased risk of ischemic stroke.1 PFO closure combined with long-term antiplatelet therapy is recommended to prevent recurrent stroke in selected patients.2
SWITCH TO THE interventional VIEW For more information specific to interventional cardiology regarding PFO closure
DURING THE PROCEDURE
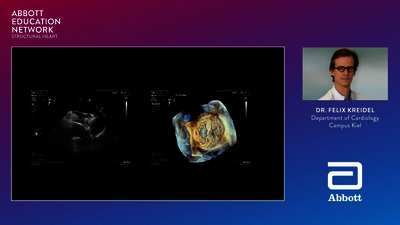
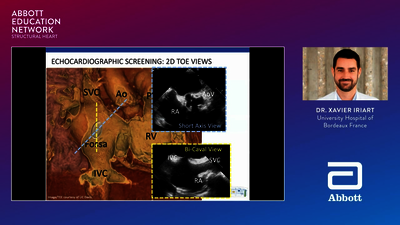
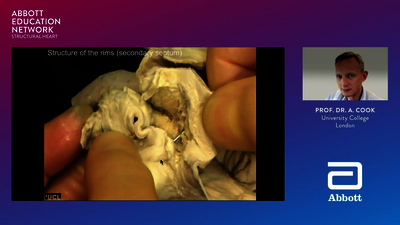
PFO closure is a minimally invasive, outpatient procedure performed under general anesthesia or conscious sedation in a heart catheterization laboratory. The catheter-based procedure involves making a very small skin incision, guided by fluoroscopy and intracardiac echocardiography, typically in the right groin area, and inserting a catheter to guide the PFO occluder through the blood vessels to close the PFO within the patient’s heart.
Once the device is placed across the PFO, the cardiologist will carefully study its position using cardiac imaging tools.
When the cardiologist is satisfied with the position of the occluder, it will be released to remain permanently in the heart. All catheters will then be removed, and the implant procedure will be complete. The procedure should last between 1 and 2 hours.
WHAT HAPPENS AFTER THE PFO CLOSURE PROCEDURE?
After the procedure, the interventional cardiologist will discuss an after-care plan with the patient. The patient can expect to be discharged from the hospital within 24–48 hours and may be prescribed aspirin (81 to 325 mg) and clopidogrel (75 mg) to be taken daily for 1 month after the implant procedure, followed by daily aspirin (81 to 325 mg) alone for at least 5 additional months. Additional medication (typically aspirin daily) may be prescribed beyond 6 months. Patients should have an echocardiogram at 6 months so the medical team can make sure that the device is properly implanted.
INTEGRATE PFO CLOSURE INTO YOUR NEUROLOGY PRACTICE WITH THIS THREE STEP PROCESS:

Identify possible candidates for closure
Perform a detailed stroke workup referencing the latest guidelines

Collaborate with an interventional cardiologist to select appropriate patients
Contact your Abbott representative to find an interventional cardiologist near you

Present PFO closure as an option to your patients
Information and resources for sharing with patients may be found on www.PFOstroke.com
Connext
Live
TV
HUB
- Kent DM, Thaler DE. Is patent foramen ovale a modifi able risk factor for stroke recurrence? Stroke. 2010;41(10 Suppl 1):S26–30. doi.org/10.1161/STROKEAHA.110.595140.
- Messé SR, Gronseth GS, Kent DM, et al. Practice advisory update summary: patent foramen ovale and secondary stroke prevention. Neurology. 2020;94(20):876–885. doi.org/10.1212/WNL.0000000000009443.
- Homma S, Sacco RL. Patent foramen ovale and stroke. Circulation. 2005;112(7):1063–1072. doi.org/10.1161/CIRCULATIONAHA.104.524371.
- Mojadidi MK, Zaman MO, Elgendy IY, et al. Cryptogenic stroke and patent foramen ovale. J Am Coll Cardiol. 2018;71(9):1035–1043. doi.org/10.1016/j.jacc.2017.12.059.
- Saver JL. Clinical practice. Cryptogenic stroke. N Engl J Med. 2016;374(21):2065–2074. doi.org/10.1056/NEJMcp1503946.
- Kernan WN, Ovbiagele B, Black HR, et al. AHA/ASA guidelines for the prevention of stroke in patients with stroke and transient ischemic attack. Stroke. 2014;45(7):2160–2236. doi.org/10.1161/STR.0000000000000024.
- Homma S, Sacco RL, Di Tullio MR, et al. E ect of medical treatment in stroke patients with patent foramen ovale: patent foramen ovale in cryptogenic stroke study. Circulation. 2002;105(22):2625–2631. doi.org/10.1161/01.CIR.0000017498.88393.44.
- Elgendy AY, Saver JL, Amin Z, et al. Proposal for updated nomenclature and classifi cation of potential causative mechanism in patent foramen ovale-associated stroke. JAMA Neurol. 2020;77(7):878–886. doi.org/10.1001/jamaneurol.2020.0458.
- Pristipino C, Sievert H, D’Ascenzo F, et al. European position paper on the management of patients with patent foramen ovale. EuroIntervention.2019;14(13):1389–1402. doi.org/10.4244/EIJ-D-18-00622.
- Diener H-C, Sacco RL, Easton JD, et al. Dabigatran for prevention of stroke after embolic stroke of undetermined source. N Engl J Med. 2019;380(20):1906–1917. doi.org/10.1056/NEJMoa1813959.