Tricuspid Regurgitation (TR) is a complex disease that has multiple causes, and is associated with high rates of morbidity and mortality.1,2 TR is highly prevalent, and among valve diseases, is one of the most undertreated.1,3 If left untreated, TR initiates a cascade of events that can lead to right-sided Heart Failure (HF) and death.4
The European Society of Cardiology/European Association of Cardiothoracic Surgery (ESC/EACTS) guidelines 2021 recommend timely referral of patients with VHD before irreversible damage occurs, and suggest that tricuspid valve interventions are underused and often initiated too late.39
Treatment of TR is guided by disease classification (primary/secondary) and severity. Typically, patients with TR are classified as having none/mild, moderate, or severe TR.22,45–47 In secondary TR, the approach to treatment is guided by the nature of the patient’s underlying heart disease.13
Current options for the treatment of TR include:

MEDICAL
MANAGEMENT

SURGICAL REPAIR
OR REPLACEMENT

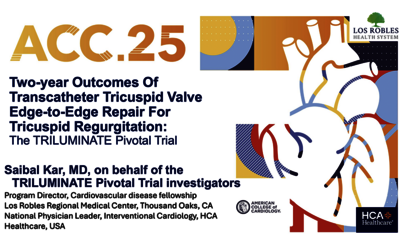
TRANSCATHETER
REPAIR
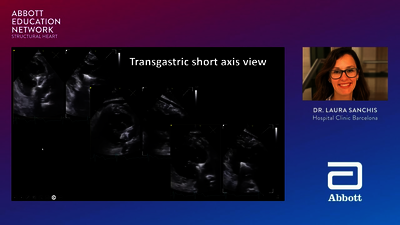
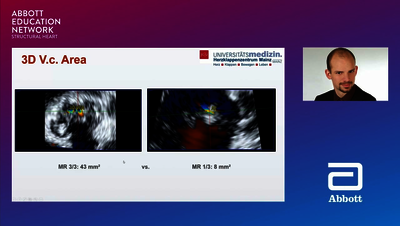
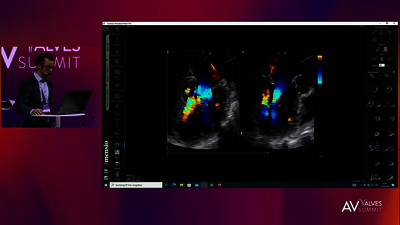
As recommended in the 2020 American College of Cardiology/American Heart Association (ACC/AHA) and 2021 ESC/EACTS guidelines,38,39 patients with TR should be managed by a multidisciplinary heart team. A heart team comprises clinical and interventional cardiologists, cardiac surgeons, imaging specialists with expertise in interventional imaging, cardiovascular anaesthesiologists, and other specialists if required (e.g. heart failure specialists, electrophysiologists).39 Comprehensive imaging includes both TTE and TEE.48
Connext
Live
TV
HUB
- Topilsky Y, Maltais S, Medina Inojosa J et al. Burden of tricuspid regurgitation in patients diagnosed in the community setting. JACC Cardiovasc Imaging. 2019;12(3):433–442. doi.org/10.1016/j.jcmg.2018.06.014.
- Taramasso M, Gavazzoni M, Maisano F. Is tricuspid regurgitation a prognostic interventional target or is it just an indicator of worst prognosis in heart failure patients? Eur Heart J. 2019;40(5):485–487. doi.org/10.1093/eurheartj/ehy722.
- Enriquez-Sarano M, Messika-Zeitoun D, Topilsky Y et al. Tricuspid regurgitation is a public health crisis. Prog Cardiovasc Dis. 2019;62(6):447–451. doi.org/10.1016/j.pcad.2019.10.009.
- Goliasch G, Mascherbauer J. Interventional treatment of tricuspid regurgitation. Wien Klin Wochenschr. 2020;132:57–60. doi.org/10.1007/s00508-020-01621-0.
- Vemulapalli S, Kerr MSD, Roberts GJ et al. Tricuspid valve disease prevalence and the impact of tricuspid valve surgery on cardiovascular events and hospital resource use in medicare beneficiaries. Am Heart J. 2022;245:100–109. doi.org/10.1016/j.ahj.2021.12.001.
- Amat-Santos IJ, Castrodeza J, Nombela-Franco L et al. Tricuspid but not mitral regurgitation determines mortality after TAVI in patients with non-severe mitral regurgitation. Rev Esp Cardiol (Engl Ed). 2018;71(5):357–364. doi.org/10.1016/j.rec.2017.08.019.
- Kammerlander AA, Marzluf BA, Graf A et al. Right ventricular dysfunction, but not tricuspid regurgitation, is associated with outcome late after left heart valve procedure. J Am Coll Cardiol. 2014;64(24):2633–2642. doi.org/10.1016/j.jacc.2014.09.062.
- Grupper A, Killu AM, Friedman PA et al. Effects of tricuspid valve regurgitation on outcome in patients with cardiac resynchronization therapy. Am J Cardiol. 2015;115(6):783–789. doi.org/10.1016/j.amjcard.2014.12.046.
- Kalbacher D, Schafer U, von Bardeleben RS et al. Impact of tricuspid valve regurgitation in surgical high-risk patients undergoing MitraClip implantation: results from the TRAMI registry. EuroIntervention. 2017;12(15):e1809–e1816. eurointervention.pcronline.com/article/impact-of-tricuspid-valve-regurgitation-in-surgical-high-risk-patients-undergoing-mitraclip-implantation-results-from-the-trami-registry.
- Nath J, Foster E, Heidenreich PA. Impact of tricuspid regurgitation on long-term survival. J Am Coll Cardiol. 2004;43(3):405–409. doi.org/10.1016/j.jacc.2003.09.036.
- Prihadi EA, van der Bijl P, Gursoy E et al. Development of significant tricuspid regurgitation over time and prognostic implications: new insights into natural history. Eur Heart J.2018;39(39):3574–3581. doi.org/10.1093/eurheartj/ehy352.
- Testa L, Latib A, De Marco F et al., editors. Euro15A-POS290: Interaction between tricuspid regurgitation and transcatheter aortic valve replacement. Insight from the Italian registry. EuroPCR; 2015; Paris, France.
- Shah PM, Raney AA. Tricuspid valve disease. Curr Probl Cardiol. 2008;33(2):47–84. doi.org/10.1016/j.cpcardiol.2007.10.004.
- Rodés-Cabau J, Taramasso M, O'Gara PT. Diagnosis and treatment of tricuspid valve disease: current and future perspectives. Lancet. 2016;388(10058):2431–2442. doi.org/10.1016/S0140-6736(16)00740-6.
- Kim SM, Singh HS, Nati J et al. Multi-modality imaging in the evaluation and treatment of tricuspid regurgitation. Curr Treat Options Cardiovasc Med. 2018;20(9):77. doi.org/10.1007/s11936-018-0672-5.
- O'Sullivan KE, Cull S, Armstrong L et al. Examining the forgotten valve: outcomes of tricuspid valve surgery, a 15-year experience. Ir J Med Sci. 2022;191(2)699–704. doi.org/10.1007/s11845-021-02608-0.
- Shiran A, Najjar R, Adawi S et al. Risk factors for progression of functional tricuspid regurgitation. Am J Cardiol. 2014;113(6):995–1000. doi.org/10.1016/j.amjcard.2013.11.055.
- British Heart Foundation. Heart Valve Disease. 2014. Available from: www.bhf.org.uk/-/media/files/publications/heart-conditions/his11_0414_heart-valve-disease_a6.pdf. Accessed on: September 2023.
- Nishimura RA, Otto CM, Bonow RO et al. 2014 AHA/ACC Guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(23):2440–2492. doi.org/10.1161/CIR.0000000000000029.
- Mayo Clinic. Tricuspid valve regurgitation. 2021. Available from: www.mayoclinic.org/diseasesconditions/tricuspid-valve-regurgitation/symptoms-causes/syc-20350168. Accessed September 2023.
- Geyer M, Keller K, Bachmann K et al. Concomitant tricuspid regurgitation severity and its secondary reduction determine long-term prognosis after transcatheter mitral valve edge-to-edge repair. Clin Res Cardiol. 2021;110(5):676–688. doi.org/10.1007/s00392-020-01798-4.
- Al-Bawardy R, Krishnaswamy A, Rajeswaran J et al. Tricuspid regurgitation and implantable devices. Pacing Clin Electrophysiol. 2015;38(2):259–266. doi.org/10.1111/pace.12530.
- Delling FN, Hassan ZK, Piatkowski G et al. Tricuspid regurgitation and mortality in patients with transvenous permanent pacemaker leads. Am J Cardiol. 2016;117(6):988–992. doi.org/10.1016/j.amjcard.2015.12.038.
- Hung J. The pathogenesis of functional tricuspid regurgitation. Semin Thorac Cardiovasc Surg. 2010;22(1):76–78. doi.org/10.1053/j.semtcvs.2010.05.004.
- Topilsky Y, Michelena HI, Messika-Zeitoun D et al. Doppler-echocardiographic assessment of tricuspid regurgitation. Prog Cardiovasc Dis. 2018;61(5–6):397–403. doi.org/10.1016/j.pcad.2018.11.008.
- Taramasso M, Pozzoli A, Guidotti A et al. Percutaneous tricuspid valve therapies: the new frontier. Eur Heart J. 2017;38(9):639–647. doi.org/10.1093/eurheartj/ehv766.
- d'Arcy JL, Coffey S, Loudon MA et al. Large-scale community echocardiographic screening reveals a major burden of undiagnosed valvular heart disease in older people: the OxVALVE Population Cohort Study. Eur Heart J. 2016;37(47):3515–3522. doi.org/10.1093/eurheartj/ehw229.
- Montalto C, Mangieri A, Jabbour RJ et al. Prevalence, burden and echocardiographic features of moderate to severe tricuspid regurgitation: Insights from a tertiary referral center. Structural Heart. 2019;3(2):123–131. doi.org/10.1080/24748706.2018.1563733.
- De la Espriella R, Santas E, Chorro FJ et al. Functional tricuspid regurgitation and recurrent admissions in patients with acute heart failure. Int J Cardiol. 2019;291:83–88. doi.org/10.1016/j.ijcard.2019.03.051.
- Lindman BR, Maniar HS, Jaber WA et al. Effect of tricuspid regurgitation and the right heart on survival after transcatheter aortic valve replacement: insights from the placement of aortic transcatheter valves II inoperable cohort. Circ Cardiovasc Interv. 2015;8(4). doi.org/10.1161/CIRCINTERVENTIONS.114.002073.
- Arsalan M, Walther T, Smith RL, 2nd et al. Tricuspid regurgitation diagnosis and treatment. Eur Heart J. 2017;38(9):634–638. doi.org/10.1093/eurheartj/ehv487.
- Ponikowski P, Voors AA, Anker SD et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology. Developed with the special contribution of the Heart Failure Association of the ESC. Eur Heart J. 2016;37(27):2129–2200. doi.org/10.1093/eurheartj/ehw128.
- Lancellotti P, Moura L, Pierard LA et al. European Association of Echocardiography recommendations for the assessment of valvular regurgitation. Part 2: mitral and tricuspid regurgitation (native valve disease). Eur J Echocardiogr. 2010;11(4):307–332. doi.org/10.1093/ejechocard/jeq031.
- De Meester P, Van De Bruaene A, Herijgers P et al. Tricuspid valve regurgitation: prevalence and relationship with different types of heart disease. Acta Cardiol. 2012;67(5):549–556. doi.org/10.1080/AC.67.5.2174129.
- Benfari G, Antoine C, Miller WL et al. Excess mortality associated with functional TR complicating heart failure with reduced ejection fraction. Circulation. 2019;140(3):196–206. doi.org/10.1161/CIRCULATIONAHA.118.038946.
- Ren Q-W, Li X-L, Fang J et al. The prevalence, predictors, and prognosis of tricuspid regurgitation in stage B and C heart failure with preserved ejection fraction. ESC Heart Fail. 2020;7(6)4051–4060. doi.org/10.1002/ehf2.13014.
- Karam N, Braun D, Mehr M et al. Impact of transcatheter tricuspid valve repair for severe tricuspid regurgitation on kidney and liver function. JACC Cardiovasc Interv.2019;12(15):1413–1420. doi.org/10.1016/j.jcin.2019.04.018.
- Otto CM, Nishimura RA, Bonow RO et al. 2020 ACC/AHA Guideline for the management of patients with valvular heart disease: Executive Summary: A report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. J Am Coll Cardiol. 2021;77(4):450–500. doi.org/10.1016/j.jacc.2020.11.035.
- Vahanian A, Beyersdorf F, Praz F et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Developed by the task force for the management of valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). European Heart Journal. 2022;43(7):561–632. doi.org/10.1093/eurheartj/ehab395.
- Zamorano JL, Badano LP, Bruce C et al. EAE/ASE recommendations for the use of echocardiography in new transcatheter interventions for valvular heart disease. Eur Heart J.2011;32(17):2189–2214. doi.org/10.1093/eurheartj/ehr259.
- Spieker M, Kelm M, Westenfeld R. Moderne Diagnostik der Mitral- und Trikuspidalklappe – was ist wirklich notwendig? Aktuelle Kardiologie. 2017;6(04):265–270. doi.org/10.1055/s-0043-115534.
- Hell MM, Achenbach S. CT support of cardiac structural interventions. Br J Radiol. 2019;92(1098):20180707. doi.org/10.1259/bjr.20180707.
- Testa L, Latib A, De Marco F et al. The failing right heart: implications and evolution in high-risk patients undergoing transcatheter aortic valve implantation. EuroIntervention.2016;12(12):1542–1549. eurointervention.pcronline.com/article/the-failing-right-heart-implications-and-evolution-in-high-risk-patients-undergoing-transcatheter-aortic-valve-implantation.
- Hahn RT, Thomas JD, Khalique OK et al. Imaging assessment of tricuspid regurgitation severity. JACC Cardiovasc Imaging. 2019;12(3):469–490. doi.org/10.1016/j.jcmg.2018.07.033.
- Badhwar V, Rankin JS, He M et al. Performing concomitant tricuspid valve repair at the time of mitral valve operations is not associated with increased operative mortality. Ann Thorac Surg. 2017;103(2):587–593. doi.org/10.1016/j.athoracsur.2016.06.004.
- Ghoreishi M, Evans CF, DeFilippi CR et al. Pulmonary hypertension adversely affects short- and long-term survival after mitral valve operation for mitral regurgitation: implications for timing of surgery. J Thorac Cardiovasc Surg. 2011;142(6):1439–1452. doi.org/10.1016/j.jtcvs.2011.08.030.
- Kelly BJ, Ho Luxford JMH, Butler CG et al. Severity of tricuspid regurgitation is associated with long-term mortality. J Thorac Cardiovasc Surg. 2018;155(3):1032–1038.e2. doi.org/10.1016/j.jtcvs.2017.09.141.
- Goldberg YH, Ho E, Chau M et al. Update on transcatheter tricuspid valve replacement therapies. Front Cardiovasc Med. 2021;8:619558. doi.org/10.3389/fcvm.2021.619558.
- McDonagh TA, Metra M, Adamo M et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2021;42(36):3599–3726. doi.org/10.1093/eurheartj/ehab368.
- Cai S, Bowers N, Dhoot A et al. Natural history of severe tricuspid regurgitation: Outcomes after transcatheter tricuspid valve intervention compared to medical therapy. Int J Cardiol. 2020;320:49–54. doi.org/10.1016/j.ijcard.2020.07.018.
- Fender EA, Zack CJ, Nishimura RA. Isolated tricuspid regurgitation: outcomes and therapeutic interventions. Heart. 2018;104(10):798–806. dx.doi.org/10.1136/heartjnl-2017-311586.
- Matli K, Mahdi A, Zibara V et al. Transcatheter tricuspid valve intervention techniques and procedural steps for the treatment of tricuspid regurgitation: a review of the literature. Open Heart. 2022;9(1):e002030. dx.doi.org/10.1136/openhrt-2022-002030.
- Besler C, Seeburger J, Thiele H et al. Treatment options for severe functional tricuspid regurgitation: indications, techniques and current challenges. ESC European J Cardiol Practice. 2018;16(31). www.escardio.org/Journals/E-Journal-of-Cardiology-Practice/Volume-16/Treatment-options-for-severe-functional-tricuspid-regurgitation-indications-techniques-and-current-challenges.
- Alqahtani F, Berzingi CO, Aljohani S et al. Contemporary trends in the use and outcomes of surgical treatment of tricuspid regurgitation. J Am Heart Assoc. 2017;6(12):e007597. doi.org/10.1161/JAHA.117.007597.
- LaPar DJ, Likosky DS, Zhang M et al. Development of a risk prediction model and clinical risk score for isolated tricuspid valve surgery. Ann Thorac Surg. 2018;106(1):129–136. doi.org/10.1016/j.athoracsur.2017.11.077.
- Wang TKM, Lim A. Isolated tricuspid valve surgery at a single centre 2001-2017 experience. Heart, Lung and Circulation. 2018;27.
- Vieitez JM, Monteagudo JM, Mahia P et al. New insights of tricuspid regurgitation: a large-scale prospective cohort study. Eur Heart J Cardiovasc Imaging. 2021:22(2):196–202. doi.org/10.1093/ehjci/jeaa205.
- Praz F, Muraru D, Kreidel F et al. Transcatheter treatment for tricuspid valve disease. EuroIntervention. 2021;17(10):791–808. eurointervention.pcronline.com/article/transcatheter-treatment-for-tricuspid-valve-disease.
- Vahanian A, Brochet E, Juliard JM. Guidelines recommendations on the treatment of tricuspid regurgitation. where are we and where do we go with transcatheter valve intervention. Front Cardiovasc Med. 2018;5:37. doi.org/10.3389/fcvm.2018.00037.
- Rodés-Cabau J, Hahn RT, Latib A et al. Transcatheter therapies for treating tricuspid regurgitation. J Am Coll Cardiol. 2016;67(15):1829–1845. doi.org/10.1016/j.jacc.2016.01.063.
- Antunes MJ, Rodriguez-Palomares J, Prendergast B et al. Management of tricuspid valve regurgitation: Position statement of the European Society of Cardiology Working Groups of Cardiovascular Surgery and Valvular Heart Disease. Eur J Cardiothorac Surg. 2017;52(6):1022–1030. doi.org/10.1093/ejcts/ezx279.
- Zack CJ, Fender EA, Chandrashekar P et al. National trends and outcomes in isolated tricuspid valve surgery. J Am Coll Cardiol. 2017;70(24):2953–2960. doi.org/10.1016/j.jacc.2017.10.039.
- Chen J, Abudupataer M, Hu K et al. Risk factors associated with perioperative morbidity and mortality following isolated tricuspid valve replacement. J Surg Res. 2018;221:224–231. doi.org/10.1016/j.jss.2017.08.014.
- Beckhoff F, Alushi B, Jung C et al. Tricuspid regurgitation – medical management and evolving interventional concepts. Front Cardiovasc Med. 2018;5:49. doi.org/10.3389/fcvm.2018.00049.
- Boyd O, Jackson N. How is risk defined in high-risk surgical patient management? Crit Care. 2005;9(4):390–396. doi.org/10.1186/cc3057.
- Minto G, Biccard B. Assessment of the high-risk perioperative patient. Continuing Education in Anaesthesia, Critical Care & Pain. 2014;14(1):12–17. doi.org/10.1093/BJACEACCP/MKT020.
- Schofer J, Bijuklic K, Tiburtius C et al. First-in-human transcatheter tricuspid valve repair in a patient with severely regurgitant tricuspid valve. J Am Coll Cardiol. 2015;65(12):1190–1195. doi.org/10.1016/j.jacc.2015.01.025.
- National Institute for Health and Care Excellence (NICE). Interventional procedures guidance [IPG731] Transcatheter tricuspid valve leaflet repair for tricuspid regurgitation. 2022. Available from: www.nice.org.uk/guidance/ipg731/. Accessed September 2023.
- Abbott Medical Devices. TriClip™ G4 System Instructions for Use 2021. Available from: vascular.eifu.abbott/en/detail-screen.html. Accessed June 2023.
- National Institute for Health and Care Excellence (NICE). Interventional procedures guidance [IPG730] Transcatheter tricuspid valve annuloplasty for tricuspid regurgitation. 2022. Available from: www.nice.org.uk/guidance/ipg730/. Accessed June 2023.
- Cardiovascular News. Cardioband becomes first-ever transcatheter tricuspid system to receive the CE mark. 2018. Available from: cardiovascularnews.com/first-ever-transcatheter-system-for-treating-tricuspid-regurgitation-approved-in-europe/. Accessed September 2023.
- Heidenreich PA, Bozkurt B, Aguilar D et al. 2022 AHA/ACC/HFSA Guideline for the management of heart failure: A report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2022;145(18):e895–e1032. doi.org/10.1161/CIR.0000000000001063.
- National Institute for Health and Care Excellence (NICE). NICE guideline [NG208] Heart valve disease presenting in adults: investigation and management. 2021. Available from: www.nice.org.uk/guidance/ng208. Accessed September 2023.