STROKE RISK FACTORS
Atrial fibrillation (AF) is associated with a 5-fold increase in the risk of ischemic stroke.1 Left atrial appendage (LAA) closure reduces the risk of stroke in non-valvular AF patients (NVAF) who are seeking an alternative to oral anticoagulants.2,3
SWITCH TO THE interventional VIEW For more information specific to interventional cardiology regarding LAA Occlusion
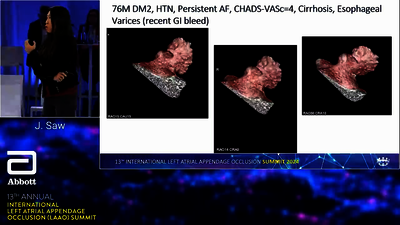
Several meta-analyses and prospective studies currently available suggest a benefit for LAAO therapy, for example in patients with intracerebral bleeding, gastrointestinal bleeding, chronic renal failure (CKD), recurrent ischemic stroke and octogenarians.
PROPENSITY SCORE MATCHED FOLLOW-UP STUDY1,2
LAA occlusion with AMPLATZER™ devices showed risk reduction over standard care
Propensity score matching of 151 patients with standard medical care to 151 consecutive LAAO patients with Amplatzer™ devices as reported in ‘Left atrial appendage occlusion versus standard medical care in patients with atrial fibrillation and intracerebral hemorrhage: A propensity score matched follow-up study.’ EuroIntervention. 2017;13(3)371–378.1
| CHARACTERISTICS (PROPENSITY SCORE MATCHED PATIENTS) | STANDARD CARE (N=147) | LAAO (N=147) |
|---|---|---|
| Age, mean (SD) | 73.3 (9.1) | 71.9 (8.7) |
| Gender (male) n (%) | 97 (66.0) | 96 (65.0) |
| CHA2DS2VASc† mean (SD) | 4.01 (1.5) | 3.9 (1.5) |
| HAS-BLED‡ mean (SD) | 4.2 (0.8) | 4.2 (0.8) |
| Antithrombotic treatment | (during follow-up) | (at latest follow-up) |
| Warfarin | 20% | 0% |
| NOAC | 23% | 0% |
| Platelet inhibitors | 37% | 71% |
| No treatment | 44% | 29% |
| CLINICAL OUTCOMES | STANDARD CARE (N=147) | LAAO (N=147) |
|---|---|---|
| Ischemic stroke/major bleeding/mortality | ||
| Events | 28 | 6 |
| Event rate (events/1000 patient-years) (95% CI) | 278.9 (229.3-339.2) | 278.9 (229.3–3 |
| Ischemic stroke | ||
| Events | 5 | 2 |
| Event rate (events/1000 patient-years) (95% CI) | 48.6 (40.1–59.0) | 15.5 (13.0–18.4) |
| Major bleeding | ||
| Events | 9 | 4 |
| Event rate (events/1000 patient-years) (95% CI) | 88.3 (72.7–107.2) | 31.7 (26.6–37.7) |
| Intracerebral hemorrhage (ICH) | 3 | 1 |
| Mortality | ||
| Events | 23 | 2 |
| Event rate (events/1000 patient-years) (95% CI) | 216.9 (179.3–262.4) | 15.4 (13.0–18.3) |
| CLINICAL OUTCOMES HR BY COX-REGRESSION ANALYSIS n=147 IN EACH PROPENSITY SCORE (PS) MATCHED PATIENT GROUP | LAAO VERSUS STANDARD CARE HAZARD RATIO (95% CI) | RELATIVE RISK REDUCTION (%) |
|---|---|---|
| Ischemic stroke/major bleeding/mortality | 0.16 (0.07–0.37)* | 81% |
| Ischemic stroke | 0.21 (0.05–1.00) | 65% |
| Major bleeding | 0.28 (0.09–0.85)* | 61% |
| Recurrent ICH | 0.10 (0.01–0.81)* | 71% |
| All-cause mortality | 0.11 (0.03–0.51)* | 92% |
- Left atrial appendage occlusion with Amplatzer™ devices showed risk reduction over standard care:
- LAAO had lower risk of composite outcome—all-cause mortality, stroke and major bleeding with relative risk reduction of 81%
- LAAO had lower risk of mortality with relative risk reduction of 92%
- LAAO reduced risk for stroke and major bleeding with relative risk reduction of 65% for stroke, 61% for major bleeding
- These study data suggest transcatheter LAAO to be a beneficial stroke prevention strategy in patients with atrial fibrillation and prior intracerebral hemorrhage
- Number Needed to Treat (NNT)—36 patients to prevent composite outcome of mortality, stroke and major bleeding, 30 patients to prevent mortality
See also ‘Clinical outcomes associated with left atrial appendage occlusion versus direct oral anticoagulation in atrial fibrillation.’
JACC Cardiovasc Interv. 2021;14(1):69–78:3
SUITABLE PATIENTS FOR LAA OCCLUSION TODAY
Until the results of the randomized studies are available, potential candidates for LAA occlusion are patients with relative or absolute contraindication for long-term anticoagulation, such as patients after intracerebral or intracranial hemorrhage, high risk of recurrent ischemic stroke, severe renal dysfunction, severe gastrointestinal bleeding or advanced age in combination with frequent falls.
INTRACRANIAL BLEEDING (ICB)4
LAAO is a safe procedure with similar procedural outcomes in patients with and without previous intracerebral bleeding
SUBSTUDY OF THE MULTICENTER COHORT REPORTED BY TZIKAS ET AL.5
- Patients with previous intracranial bleeding were more frequently on single acetylsalicylic acid therapy after LAAO (42.4% versus 28.3%)
- Average follow-up of 1.3 years
- The observed annual stroke/transient ischemic attack (TIA) rate for patients with previous ICB was 1.4% (75% relative risk reduction)
- The observed annual major bleeding rate (procedure and follow-up) for patients with previous ICB was 0.7% (89% relative risk reduction)4
OCTOGENARIANS
Left atrial appendage occlusion may be safe and efficacious for stroke prevention in elderly AF patients and LAAO should not be discouraged on the basis of age.9,10
75 PATIENT COHORT STUDY9 AGED 80+ WITH LAAO
- 44% not taking OAC despite high CHADS2, CHA2DS2VASc†
- Absence of TIA/cerebrovascular accident (CVA) = 98.7% at 1 year9
SUBSTUDY OF THE MULTICENTER COHORT REPORTED BY TZIKAS ET AL.8
Found similar major adverse event rates between patients < 75 years and ≥ 75 years of age, although the rate of cardiac tamponade was significantly higher in older patients
- Similar reductions in stroke compared to expected rates (stroke reduction: < 75 years = 69% versus ≥ 75 years = 74.9%)
- Similar reductions in bleeding compared to expected rates (bleeding risk reduction: < 75 years = 75.5% versus ≥ 75 = 69.2%)10
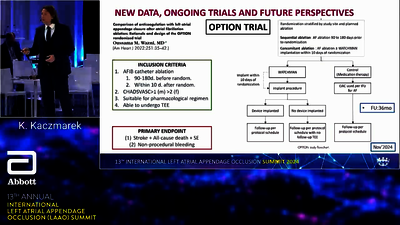
ONGOING STUDIES WITH THE AMPLATZER™ AMULET™ DEVICE
In order to advance the current guidance on how to manage patients with OAC treatment failure, more randomized controlled trials (RCTs) are needed to confirm the findings of the latest analyses.
CLOSURE-AF
STUDY OVERVIEW
DESIGN
PRIMARY ENDPOINT
STUDY SPONSOR & LINK
The study goal is to determine the clinical benefit of percutaneous catheter-based left atrial appendage (LAA) closure in patients with non-valvular atrial fibrillation (NVAF) at high risk of stroke (CHA2DS2VASc† score ≥2) as well as high risk of bleeding as compared to best medical care (including a [non-vitamin K] oral anticoagulant [(N)OAC] when eligible).
Prospective 1512 patients, randomized to LAAO and to medical therapy followed for 2 years.
Primary endpoint (net clinical benefit) [time frame: follow-up: 24 months.] Survival time free of the composite of:
- Stroke (including ischemic or hemorrhagic stroke)
- Systemic embolism
- Major bleeding: Bleeding Academic Research Consortium (BARC) type 3–5
- Cardiovascular or unexplained death
Study sponsor: Charité University, Berlin, Germany
STROKECLOSE STUDY
STUDY OVERVIEW
DESIGN
PRIMARY ENDPOINT
STUDY SPONSOR & LINK
The aim of STROKECLOSE is to assess the effect of LAAO to reduce the incidence stroke, bleeding and cardiovascular mortality in patients with NVAF and prior ICH.
A multicenter prospective randomized open-label clinical trial with blinded outcome evaluation (PROBE design) and blinded safety outcome assessment. The active comparison LAAO is tested against medical therapy in a 2:1 stratified randomization.
Composite endpoint of stroke (ischemic or hemorrhagic), systemic embolism, life-threatening or major bleeding and all-cause mortality [time frame: up to 5 years after randomization.] This endpoint will be assessed in patients with paroxysmal, persistent or long-standing NVAF and with ICH within 6 months prior to enrollment. The effect of LAAO will be compared to medical therapy at the treating physician’s discretion as a control.
Study sponsor: Karolinska University Hospital
CATALYST STUDY
STUDY OVERVIEW
DESIGN
PRIMARY ENDPOINT
STUDY SPONSOR & LINK
The objective of this trial is to evaluate the safety and effectiveness of the Amulet™ LAA Occluder compared to NOAC therapy in patients with non-valvular AF at increased risk for ischemic stroke and who are recommended for long-term NOAC therapy. The clinical investigation is a prospective, randomized, multicenter active control worldwide trial. Subjects will be randomized in a 1:1 ratio between the Amulet™ LAA occlusion device (“device group”) and a commercially available NOAC medication (“control group”). The choice of NOAC in the control group will be left to study physician discretion.
Prospective, randomized, multicenter active control worldwide trial.
- Composite of ischemic stroke, systemic embolism, or cardiovascular (CV) mortality (non-inferiority)
- Major or clinically relevant non-major bleeding (non-inferiority)
- Major or clinically relevant non-major bleeding, excluding procedure related events (superiority)
Study sponsor: Abbott Medical Devices
FIND OUT MORE ABOUT AMULET™ OCCLUDER DATA:
AMULET IDE 5 YR ONE-PAGER AMULET IDE 5 YR PUBLICATION CONCOMITANT EMERGE STUDY OBSERVATIONAL STUDY
CHA2DS2VASc SCORE TOOL6
| CONDITION | POINTS | |
|---|---|---|
| C | Congestive heart failure | 1 |
| H | Hypertension | 1 |
| A2 | Age ≥ 75 years | 2 |
| D | Diabetes mellitus | 1 |
| S2 | Stroke/Transient ischemic attack (TIA) | 2 |
| V | Vascular disease | 1 |
| A | Age 65–74 years | 1 |
| Sc | Sex category (female) | 1 |
HAS-BLED SCORE TOOL2
| CONDITION | POINTS | |
|---|---|---|
| H | Hypertension | 1 |
| A | Renal/liver dysfunction | 1 or 2 |
| S | Stroke | 1 |
| B | Bleeding | 1 |
| L | Labile international normalized ratios (INRs) | 2 |
| E | Elderly (age > 65 years) | 1 |
| D | Drugs or alcohol abuse | 1 or 2 |
FIND OUT MORE ABOUT AMULET™ OCCLUDER DATA:
TV
TV
- Nielsen-Kudsk JE, Johnsen SP, Wester P, et al. Left atrial appendage occlusion versus standard medical care in patients with atrial fibrillation and intracerebral hemorrhage: A propensity score matched follow-up study. EuroIntervention. 2017;13(3)371–378. doi.org/10.4244/EIJ-D-17-00201.
- Gloekler, S. 2017. Percutaneous LAAO vs. OAC: A propensity score matched study of 1000 patients with atrial fibrillation. Presented at EuroPCR, Paris May 2017.
- Nielsen-Kudsk JE, Korsholm K, Damgaard D,et al. Clinical outcomes associated with left atrial appendage occlusion versus direct oral anticoagulation in atrial fibrillation. JACC Cardiovasc Interv. 2021;14(1):69–78. doi.org/10.1016/j.jcin.2020.09.051.
- Tzikas A, Freixa X, Llull L, et al. Patients with intracranial bleeding and atrial fibrillation treated with left atrial appendage occlusion: Results from the AMPLATZER Cardiac Plug registry. Int J Cardiol. 2017; 236:232–236. doi.org/10.1016/j.ijcard.2017.02.042.
- Tzikas A, Shakir S, Gafoor S, et al. Left atrial appendage occlusion for stroke prevention in atrial fibrillation: multicentre experience with the AMPLATZER Cardiac Plug. EuroIntervention. 2016;11(10), 1170–1179. doi.org/10.4244/EIJY15M01_06.
- Gafoor S, Franke J, Bertog S, et al. Left atrial appendage occlusion in octogenarians: short-term and 1-year follow-up. Catheter Cardiovasc Interv. 2014;83(5):805–810. doi.org/10.1002/ccd.25297.
- Freixa X, Gafoor S, Regueiro A, et al. Comparison of efficacy and safety of left atrial appendage occlusion in patients < 75 to ≥ 75 years. Am J Cardiol. 2016;117(1), 84–90. doi.org/10.1016/j.amjcard.2015.10.024.
- European Heart Rhythm Association; European Association for Cardio-Thoracic Surgery; Camm AJ, Kirchhof P, Lip GY, et al. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur Heart J. 2010;31(19):2369–429. doi.org/10.1093/eurheartj/ehq278. Erratum in: Eur Heart J. 2011;32(9):1172. PMID: 20802247.